Environmental Control Unit for MCS
Environmental physicians operated special hospital wards for people with environmental illnesses from the 1970s and into the 1990s.
Keywords: environmental control unit, environmental unit, ecology unit, isolation, hospital ward, chemical sensitivity, MCS, Theron Randolph, William Rea, history
The need for an environmental isolation unit
The pioneer of environmental medicine, Dr. Theron Randolph, realized in the early 1970s that many of his severe patients were so sick that it was impossible to determine what caused their symptoms. They were chronically ill from the many things they were exposed to in their homes, their work and in the foods they ate.
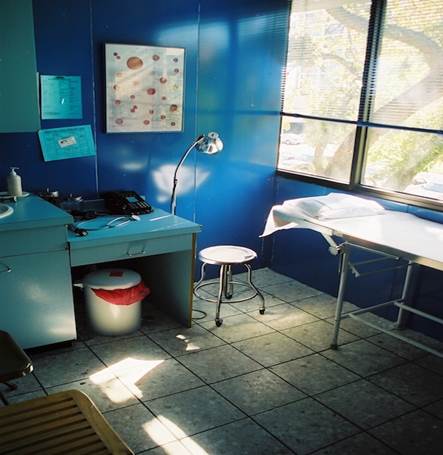
Some rooms had porcelain-on-steel walls and terrazzo floors. This
picture is from Dr. Rea’s clinic in 1999, which looked similar to his ECU.
It was not possible to test them in an office, since the test partly relied on the patient reporting whether their symptoms got worse or not.
There was a need to completely isolate the patients from their daily environment in a place that had as few triggers as possible. The result was the Environmental Control Unit (ECU).
Randolph’s first attempt of creating an ECU was not successful, and it was never opened. The first ECU was opened by Dr. Lawrence Dickey in Colorado, with Randolph’s second attempt opening in 1975. Dr. William Rea also opened his first ECU in Dallas in 1975.
Dr. Rea had a succession of four ECUs that replaced each other; his last was at TriCity Hospital it was closed in 1998 and was possibly the last ECU to operate.
Other ECUs operated in Australia, Canada, China, Germany and Great Britain as well as several places in the United States. They are listed later in this article.
The Environmental Control Unit
The ECU was designed to have as pristine air as possible. It was usually a floor in a hospital that was isolated from the rest of the building. This isolation was necessary, since fumes from fragrances, cleaning products and cigarette smoke would otherwise waft in. (Yes, people smoked inside hospitals in those days.)
They had to seal off ventilation shafts, cable shafts and elevator shafts. The ventilation channels were blocked off. They used large air cleaners made of stainless steel.
The entrance from the rest of the hospital had two sets of double doors to act as an airlock. Inside the air lock was a big air cleaner to combat fumes rolling in when the doors were opened.
In Dr. Rea’s Brookhaven ECU there were two sets of double doors into a vestibule, then another two sets of double doors going into the hallway where the patient rooms were.
There were no carpets and nearly no plastics of any kind in the unit. The floor was covered with tile or stone. The walls were aluminum, plaster, tile or porcelain-on-steel. In some ECUs the rooms were made with different materials, so the patients could choose which material worked best for them.
The furniture was made of steel, aluminum, wood, wool, leather and cotton. No synthetic foam pads, rubber or plastic.
The staff used no makeup, hair spray or fragrances. Some of them were environmentally ill themselves, having here found a place they were able to hold a job. Warning signs were posted on the door and visitors were screened to be sure they had no smell on them.
The food was organic and made from scratch in the unit’s own kitchen. Drinking water came in glass bottles from pristine sources.
Books and newspapers were kept sealed up in reading boxes, so the fumes didn’t make people sick.
The patients typically stayed for three weeks, during which time they never went outside the unit. When they arrived they were stripped of any synthetic clothing, plastic suitcases, cosmetics and other problematic substances.
Randolph (1990) tells the story that when his ECU opened, some patients were so sensitive to pesticides that they had to replace some baseboards and old flooring, since they had been sprayed for bugs years before.
This all happened before the big rollout of mobile phones and their towers, which happened in major American cities in 1996 and 1997. As many people with severe MCS also have electrical sensitivities, electropollution is a factor that today also has to be controlled.
Testing
In this rigidly controlled environment, most patients would become clear of chronic symptoms and could then discover what caused them.
Initially they fasted for up to five days, so symptoms caused by foods could clear.
Then they tested various sources of water to find which agreed with them the most. These tests included the local chlorinated city water, as well as several brands of spring water available in glass bottles.
Water was never served in plastic bottles. Some brands of water were available in both plastic and glass bottles, which were analyzed by a laboratory to document that plastic leached out into the water (Rea, 2002).

Water was served in glass bottles from pristine sources.
The doctors found that many patients got symptoms from drinking the city water, and some even from certain spring waters.
Then the patients tried eating a variety of basic foods, one ingredient per meal, so they could monitor their symptoms. These meals were all organic. When they had discovered what foods they were allergic to, then they retested the “safe” foods, but this time using regular store-bought foods – i.e. foods treated with pesticides or stored in plastic-lined cans, to see if they caused symptoms.
The meals were cooked in the ECU’s own dedicated kitchen, using pots of stainless steel or glass and on an electric stove. These precautions were necessary to eliminate as many sources of pollution as possible.
They could also expose the patients to various chemicals in a controlled manner. In a separate room they kept sealed glass jars with samples of carpets, carbonless copy paper and many other things that the patients could sniff and see if it made them sick. They also had a gas burner to simulate the fumes from a gas stove.
In some ECUs the testing was done single-blinded, i.e. the patient did not know what the chemical was, or whether it was a blank (placebo). Full double-blinded testing was rarely done, since it was more expensive to do.
In some ECUs the smell-testing was apparently not blinded, i.e. the patient knew what they were testing, which is less reliable. They were focusing on helping patients, not writing research papers.
For more details on operating an ECU see (Randolph, 1990; Selner, 1986; Temple, 1980).
When the patients were released, they were given detailed instructions on what foods they should avoid and how to clean up their homes. For those people with many food allergies, there were instructions on how to rotate the foods so they ate them only once every four days to control their food allergies. (Some food allergies go away if limiting the exposures for several months.)
Surgical Ward
People with MCS get the same medical problems other people do. Sometimes they need surgery, but regular hospitals tend to ignore the special needs of the chemically sensitive.
Dr. Rea was also a surgeon and many people with MCS travelled to Dallas for surgery, so their environmental needs could be met. Some of them stayed in Dr. Rea’s ECU to recuperate afterwards.
Research ECUs
The purpose of the regular ECUs was to treat the patients. Their purpose was not to do research, which requires additional funding. It is not fair to patients that they should pay for research besides their treatment.
Smaller studies were done by Drs. Rea and Randolph in their ECUs, but there was a need for an ECU that was focused on research and which had funding for it. Such an ECU could have even more stringent controls so placebo effects could be ruled out.
Since much of the medical establishment was strongly opposed to accepting that MCS was real, the facility should be operated by someone neutral in the heated debate.
Unfortunately, such an ECU was never built, but it almost happened.
The U.S. Congress and U.S. Department of Veterans Affairs allocated $1.2 million to build and operate an ECU in 1994. It was supposed to be built at a university and have four patient rooms with a total of eight beds (Twombly, 1994; Ashford, 1998: ch 8).
The money was never released, so the research ECU was never built. The reason the money was withheld was never revealed (Ashford, 1998: ch 8).
It is easy to speculate that politics got in the way. Powerful special interests much preferred that MCS was kept controversial and never became accepted as legitimate. These forces were very active in the 1990s.
Other scientists attempted to get funding for scientific studies, using existing ECUs, but they were given the run-around and denials (Meggs, 2017).
The opposition builds an ECU
All the ECUs were operated by physicians who accepted MCS as a legitimate illness, as far as we have been able to find out. With one exception: Psychiatrist John Selner built an ECU at Presbyterian-St. Luke Hospital in Denver,
Colorado in 1979 (Ashford, 1998: ch 2; Selner, 1986; Staudenmayer, 1993).
Together with psychologist Dr. Herman Staudenmayer, Dr. Selner treated MCS patients in his ECU for a number of years. Their fundamental paradigm was that MCS was a psychiatric illness, though they did report cases where they had to admit the symptoms were caused by chemicals the patient was not aware of (Selner, 1986).
They published several articles that were mostly opinion pieces, where they attacked the legitimacy of MCS. In one, they claimed they could “deprogram” MCS patients who were sufficiently “receptive” (Selner, 1988), but never published any documentation for these claims (Ashford, 1998: ch 8).
The two scientists publicly spoke out against accepting MCS at conferences and in newspaper articles (Logue, 1992; Epstein, 1994; Carruthers and Staudenmayer, 1996).
The end of the ECUs
Dr. Randolph had more than ten thousand patients come through his unit in Chicago from 1975 and until he closed it in the late 1980s. He had to close because it was too expensive to run and the medical insurers refused to pay for the patients to stay there (Randolph, 1990).
The last unit to close was apparently Dr. Rea’s at TriCity Hospital in Dallas. After having no ECU for about a decade, he operated this one for about a year but had to close it in 1998.
Patients were then tested in special clinics as outpatients. Some clinics operated special apartments that were modified and rented to out-of-town patients. In Dallas entrepreneurs opened multiple housing projects to serve patients at Dr. Rea’s clinic. Besides Dr. Rea’s own housing, there was Sprague House, Raintree, Ecology Housing and Regina Caelis (apartments and cottages).
List of environmental control units
We have identified a total of 16 environmental control units in six countries. Most of them we know virtually nothing about, except they existed at some point.
|
Country |
City |
Location |
Physician |
Comment |
|
Australia |
Melbourne |
|
Little |
Opened 1992 |
|
Canada |
Halifax |
|
Fox |
|
|
China |
Beijing |
Peking Union Medical School |
Zang |
|
|
Germany |
Bad Emstal |
|
Runow |
|
|
Germany |
|
|
Stemman |
|
|
Great Britain |
London |
Nightingale Hospital |
Monro |
|
|
Great Britain |
Midlands |
|
Maberly |
|
|
United States |
Chicago/Zion |
|
Randolph |
Opened 1975 |
|
United States |
Chicago |
Henrotin Hospital |
Randolph |
Randolph’s second ECU |
|
United States |
Dallas |
Brookhaven Med Ctr |
Rea |
Opened 1975, 20 beds |
|
United States |
Dallas/Bedford |
Northeast Community H. |
Rea |
1984-1987 |
|
United States |
Dallas/Carrollton |
Carrollton Community H. |
Rea |
1982-1983 |
|
United States |
Dallas/Mesquite |
TriCity Hospital |
Rea |
1997-1998 |
|
United States |
Denver |
Presbyterian-St. Luke Hospital |
Selner |
Opened 1979 |
|
United States |
Fort Collins, Co |
|
Dickey |
First ECU |
|
United States |
Los Angeles, CA |
City View Hospital |
Stavish |
Opened 1981, 11 beds |
|
United States |
Watertown, SD |
|
|
|
|
United States |
Whiteville, NC |
|
|
|
Sources and references
Ashford, Nicholas and Claudia Miller. Chemical exposures – low levels and high stakes (second edition), New York: John Wiley and Sons, 1998.
Carruthers, Garrey and Herman Staudenmayer. Analyze syndrome before making policy (op-ed), Albuquerque Journal, July 6, 1996.
Conoley, Gillian. Living may be hazardous to your health, American Way, February 1980.
Duty, Juana E. Pasadena clinic treats people allergic to environment, Los Angeles Times, January 1, 1982.
Epstein, Keith. $1.8 million buys 11 units for ‘sensitive’ Californians, Cleveland Plain Dealer, July 19, 1994. Front page.
Hickey, Ellie (Dr Rea’s secretary). Personal information, March 11, 2022.
Krier, Beth Ann. A woman allergic to almost everything, Los Angeles Times, September 8, 1978
Logue, Mayada. Trip report: symposium on multiple chemical sensitivities (internal Philip Morris memo), November 24, 1992. PMDocs archive.
Meggs, William. History of the rise and fall of environmental medicine in the United States, Ecopsychology, 9, June 2017.
Randolph, Theron and Ralph Moss. An alternative approach to allergies (revised edition), New York: Harper and Row, 1990.
Rea, William. Optimum environments for optimum health and creativity, Dallas, TX: Crown Press, 2002.
Rea, William. History of chemical sensitivity and diagnosis, Reviews of Environmental Health, 2016.
Selner, John. Chemical sensitivity, Current Therapy in Allergy, Immunology and Rheumatology, 3, 1988.
Selner, John and Herman Staudenmayer. The relationship of the environment and food to allergic and psychiatric illness, In Psychobiological aspects of allergic disorders, edited by Young, Rubin and Daman, New York: Praeger, 1986.
Staudenmayer, Herman, John Selner and Martin Buhr. Double-blind provocation chamber challenges in 20 patients presenting with “multiple chemical sensitivity,” Regulatory Toxicology and Pharmacology, 18, 44-53, 1993.
Temple, Truman. On the cutting edge, EPA Journal, October 1980.
Twombly, Renee. MCS: a sensitive issue, Environmental Health Perspectives, 102, September 1994. (see sidebar: Gulf War Veterans.)
This author has visited Dr. Rea’s clinic in Dallas, but not any of his ECUs. Also, we talked to an MCS patient who stayed at Dr. Rea’s ECU at Brookhaven in 1979 for five weeks and some years later at another of his ECUs to recuperate after surgery (he wishes to remain anonymous).
More Information
More MCS history is available on www.eiwellspring.org/history.html
2021 (updated 2023)