Introduction to Electrical Hypersensitivity
People who have electrical hypersensitivity (EHS) get symptoms from exposures to electromagnetic radiation at levels far below legal limits, such as from computers, electric stoves, mobile phones, electric wires, and many other types of electronics and electrical equipment. The disease is controversial and poorly understood; research is still in its infancy and starved of funding.
Keywords:��� electrical sensitivity, electromagnetic hypersensitivity, EHS, electromagnetic sensitivity, electromagnetic fields, EMF, electromagnetic radiation, sickness, symptoms, diagnosis, children
This is for informational purposes only and not intended to provide advice on diagnosis, treatment or other medical aspects. If you think you have EHS, please consult a physician with experience in this illness.
We use the term EHS here, as that is the one most commonly used throughout the world, both in the patient communities, newspapers, and the scientific journals. There are other terms used, such as �idiopathic environmental intolerance� which tends to be used by people who are focused on labeling EHS as purely psychological (often along with multiple chemical sensitivity). Another is �electromagnetic sensitivity,� though its acronym (EMS) is confusing since in the medical world it stands for �emergency medical service,� i.e. an ambulance team.
Symptoms
The symptoms of EHS are usually neurologic, and can affect many parts of the body. They vary from person to person; few have all the listed symptoms. Common symptoms include:
� Tingling or burning skin, without redness (paresthesia)
� Ringing in the ears (tinnitus)
� Headaches
� Restlessness, irritability
� Dizziness, problems concentrating
� Sleep problems
� Chest discomfort
� Fatigue
� Joint pain/muscle pain
Many other symptoms have been reported, including irritable bowels, skin lesions, facial flushing, racing heart (tachycardia), anxiety, depression, eye symptoms (pain, vision disturbances), memory problems, light sensitivity, sound sensitivity and more (FEB 2007; Genuis 2011; Baliatsas 2014; Hedendahl 2015; Belyaev 2016; Belpomme 2020).
People with severe EHS sometimes report sensations of heat or tingling in their feet or hands or face.
None of these symptoms are specific to EHS; they can all have other causes.
Complex sensitivities
EHS appears to be a spectrum disease, where the sensitivities and symptoms can vary widely. Other examples of spectrum diseases are Covid-19, autism, and migraines.
Small pioneering studies done in Britain in the late 1980s, and a major study by William Rea (Rea 1991) show that people with EHS tend to be sensitive to some frequencies, but not all (Genuis 2011). This is similar to people with pollen allergies, who are reactive to some pollen but not all pollen (EHS is not an allergy).
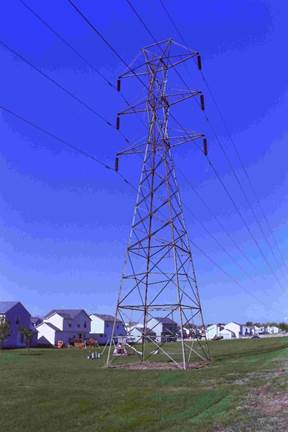
This may explain why some people are sensitive to some types of electronics and not others (FEB 2007; Eltiti 2007; De Luca 2014; Hojo 2017). Anecdotally, this writer has met people from Europe who were bothered by power lines there, but not in the United States. The reason could be the different frequencies (50 cycles versus 60 cycles).
Once a person has become sensitized, the symptoms tend to become worse over time if the exposures continue. It is thus a bad idea to try to tough it out, as that can have a lasting effect. Early intervention may halt further progression of EHS (there are no studies documenting this).
Many types of electronics generate several frequencies at the same time, which may be a reason they are a problem for so many people with EHS. Examples are mobile phones, computers and electric cars. (A mobile phone emits a carrier frequency, modulations and pulses of the carrier, plus several internal frequencies from voltage converters, microprocessors, etc).
Some people have symptoms within a couple of minutes of an exposure, while others will first have them later � sometimes even hours after the exposure ended. There is sometimes an adaptation effect where symptoms eventually stop during prolonged exposure and then reappear much later.
A major exposure may cause symptoms to last for days, and the person may have heightened sensitivity for some days or even weeks. This is similar to when skin is burned or broken, where the wounded place will be more sensitive for a while.
Tinnitus is a common symptom (Nordin 2014). The prominent EHS physician William Rea has speculated that exposure to EMF may cause swelling inside the head that presses on the auditory nerve (personal communication).
In rare cases people with EHS can actually �hear� low levels of electromagnetic radiation (Wieske 1963; Firstenberg 2017; Belkin 1990). At high radiation levels most people are able to �hear� microwaves, which is called the �Frey effect� or �RF hearing� (Frey 1962; Elder 2003).
Light sensitivity is common. Thirteen to 45 percent of people with EHS also report sensitivity to light (FEB 2007; Schooneveld 2007; Kato 2012). It is unclear how many are sensitive to bright light and how many have problems with specific colors (bluish light seems to be a particular problem). A few become so sensitive they cannot go outdoors during daytime (Johansson 1999).
Sensitivity to sunlight (or perhaps the many other frequencies emanating from the sun) may be a reason why many people with EHS feel better at night, even to the point where some normally stay up past midnight. However, many also report that they are more sensitive to electromagnetic radiation when trying to sleep at night.
These daily cycles have not been investigated scientifically, though already the fifth century Roman physician Caelius Aurelianus noted that asthma attacks were more common at night (Greenwood 2018).
Sensitivity to flickering lights may also be common. Computers, televisions and fluorescent lights are some of the most commonly reported problems (FEB 2007). Those three all emit flickering light, which may be a contributing factor to the symptoms people report. Swedish scientists exposed ten people with EHS to flashing lights in a low-EMF room, while measuring their brain waves. Their brain responses were distinctly higher than for the ten people without EHS they also tested (Sandstrom 1997). This was further explored by the same scientists (Lyskov 2001).
Some people with EHS are also sensitive to sound (Solberg 2010; Nordin 2014; Palmquist 2013; Hillert 2002). Anecdotally it appears to be especially a problem with complex sounds, such as music, and low-quality sound, such as from telephones.
Skin problems are common, especially dermatitis/eczema (De Luca 2014). In some cases the face can be flushed after using a computer or television.
A small percentage of EHS patients show skin effects, such as flushing or lesions. They mostly happen in the face or on the hands (Belpomme 2020).
A German pilot study showed that people with EHS have modified nerve signals when exposed to wireless (Wi-Fi) signals, with the effect lasting some time after the exposure (von Klitzing 2021).
It appears that people with EHS get sensitized to whatever frequencies they are exposed to frequently. In practice that means that a new piece of home electronics many cause no problems for a while, but eventually it does. This is also similar to pollen allergies, where people who move to a different climate may get relief from their allergies, but eventually become allergic to the local pollen. (EHS is not an allergy, we just use allergies as a familiar illustration.)
Metal implants may be a factor, as they can absorb, reradiate, and reflect radio waves, and thereby cause stronger levels in tissue in contact with the metal. In one of her books about EHS, Swedish journalist Gunni Nordstrom writes about a man who had a titanium plate installed in his jaw. He could not tolerate using a mobile phone until the plate was removed again (Nordstrom 2000).
The Environmental Health Trust web site (ehtrust.org) lists multiple studies involving eyeglasses, jewelry, and metal implants.
Diagnosing EHS
It is difficult to diagnose EHS, as there are no objective lab tests available yet and the symptoms can all have other causes. For instance, tinnitus can also be caused by metabolic deficiencies, mercury, lead, and several types of drugs (Wikipedia).
A physician will tend to diagnose EHS based on patient history and by eliminating other possible illnesses (Belyaev 2016).
There are physicians who are trying to put together more specific diagnostic procedures (Belyaev 2016; Belpomme 2020; Heuser 2017; Austrian Medical Association 2012), but no consensus yet.
The most promising work has been done in France, using ultrasonic brain scans (Belpomme 2020; Irigaray 2018a; Greco 2020).
Biomarkers for oxidative stress have also been found (Irigaray 2018b).
The illness is controversial, and few physicians can actually diagnose it. In the United States, these specialists are organized in the American Academy of Environmental Medicine, which has a referral service on their website. In other countries a local EHS support group may provide a referral.
Some people are not able to find a specialist or afford one. Trying to self-diagnose can be perilous as it may not be correct. An incorrect diagnosis can result in unnecessary life disruption, financial hardship, and that the real illness is not addressed. Computers are a common source of symptoms, but is it the radiation that causes it, or the chemical fumes? Or simply eyestrain? Be skeptical of your own findings, don�t jump to conclusions.
A common way to experiment is to fully turn off all portable electronics and as many breakers as possible before going to bed at night. Then sleep in a room away from the refrigerator, electric meter and other things still left on. Be aware that walls do not really block radiation, including from next-door neighbors. If you live in an apartment, it may not be possible to lower the radiation level enough to notice. An alternative is to go camping in a rural area with no electrical service, no nearby transmitters or houses, and no portable electronics at all. Or rent a primitive cabin.

Do multiple tests to see if you feel better. Be aware that a relaxing camping trip may make you feel better even if you don�t have EHS.
Another method is to keep a diary of symptoms and activities for a few weeks, and then go over it in detail to see if there is a pattern. This is especially helpful if the symptoms first appear some time after the exposure, or only certain exposures are a problem.
Experimenting by exposing yourself to electrical things is not reliable. You may simply get symptoms because you expect to (called placebo/nocebo effect). Even if you have a friend turn things on or off without your knowing, this effect still makes such testing unreliable. People with EHS tend to have good days and bad days with symptoms that come and go for unknown reasons. This makes such testing very difficult.
Exposing someone to radiation without their consent is unethical and a serious breach of trust that can permanently damage a relationship. It is also not a reliable method (see later).
Diagnostic codes
In some countries, physicians are recommended to use ICD-10 code R68.8 together with Z58.4 and codes for the specific symptoms (Belyaev 2015).
What causes EHS?
The cause of EHS is not known and hotly debated (Belyaev 2016; Genuis 2011). It may be that some people�s bodies are more susceptible to the ever-increasing electromagnetic radiation we are all exposed to.
Some people report their first symptoms from using computers or mobile phones, but that does not prove they caused the illness. EHS existed before mobile phones and computers, though it was very rare then. The first rise in cases happened in the 1980s when many businesses installed computers on people�s desks.
Humanity has lived with very low levels of electromagnetic radiation until recent decades. This author has measured the ambient microwave levels in remote areas to be below 0.001 uW/m2. In the late 1970s, the U.S. Environmental Protection Agency did extensive measurements in 15 large cities and found the median exposure level was 50 uW/m2 (Tell 1980).
Twenty years later, in 1999-2000, Swedish scientists found levels between 8 and 300 uW/m2 in a large city (and 0.07 to 40 uW/m2 in villages). (Uddmar 1999, 2000.)
Measurements in today�s cities show radiation levels that are often above 3000 uW/m2 and occasionally exceed 100,000 uW/m2 in both public places and private homes (Hardell 2017b, 2018a, 2018b; Nilsson 2023).
Today�s cities expose people to radiation that is about a million times stronger than remote areas. Occasionally it is a hundred million times stronger. It may simply be we have exceeded what some people can handle.
A possibility is that since electromagnetic radiation can make the blood-brain barrier leaky (Persson 1997; Eberhardt 2008), exposures to both EMF and neurotoxic chemicals at the same time may be a factor (Hardell 2008; Belpomme 2015). Computers may be a culprit, since they both radiate microwaves and offgas toxic chemicals (Bako-Biro 2004).
There is some evidence that EHS may be an autoimmune disease, attacking the nervous system (Belpomme 2020).
Mercury released from dental fillings when exposed to electromagnetic fields may be a factor (Mortazavi 2014).
Oxidative stress may also be a cause (Irigaray 2018b).
There is also a theory involving the calcium channels in the human cells (Pall 2013, 2016). Another theory is about mast cells (Gangi 2000).
The human brain contains microscopic magnets (Kirschvink 1996). The same types of magnets are used by migratory birds for navigation, which can be confused by radio towers (Engels 2014).
People with EHS tend to have an autonomous nervous system that is out of balance (Lyskov 2001). Whether that is a cause or an effect of the illness in unknown.
There are several other hypotheses (Belyaev 2016; Genuis 2011).
There may be a genetic factor, as about 20% of people with EHS report that a close family member also has the illness (FEB 2007; Schooneveld 2007).
Actual genetic studies of people with EHS are very scarce (De Luca 2014).
Clarity regarding EHS is likely to take decades yet. This continues to leave those suffering from the illness in limbo regarding treatments, accommodations, insurance coverage, and disability acceptance. This is similar to other ill-defined diseases, such as multiple chemical sensitivity, post-Lyme disease, chronic fatigue syndrome (CFS/ME) and others (Cara 2017; Haas 2018).
Overlap with other diseases
There seem to be overlaps with some other illnesses, most of which are also poorly understood. Lack of research funding means this area is mostly uncharted.
Multiple chemical sensitivity (MCS) is a hypersensitivity to many chemicals, such as fragrances, pesticides, paints, exhaust fumes, printed materials, and more. As for EHS the symptoms are diverse and vary with the person. The two diseases also share a variety of symptoms, such as headaches, memory problems, problems concentrating, dizziness, and fatigue (McCampbell 2011; Belpomme 2020).
In six studies, people who reported they had MCS were asked if they also believed they had EHS.
|
United States |
32% |
LeRoy 1996 |
|
United States |
8% |
Levallois 2002 |
|
Italy |
35% |
De Luca 2011 |
|
Sweden |
7% |
Palmquist 2013 |
|
Spain |
52% |
Loria-Kohen 2017 |
|
Japan |
14% |
Watai 2018 |
People with MCS who also report EHS.
The large variety may be due to the selection of people. De Luca and Loria-Kohen asked patients at MCS clinics, which tend to have more severe MCS. It thus appears that people with severe MCS are more likely to also have EHS.
In these studies, people who reported they had EHS were asked if they also had MCS:
|
United States |
60% |
Levallois 2002 |
|
Sweden |
33% |
Palmquist 2013 |
|
Japan |
76% |
Kato 2012 |
|
Italy |
95% |
De Luca 2014 |
|
Japan |
40% |
Hojo 2016 |
|
France |
23% |
Belpomme 2020 |
People with EHS who also report MCS.
The large variance may be due to what population was asked. Most of these studies were patients at clinics.
A study by professor Dominique Belpomme in France found eleven biomarkers that might be used for diagnosing both MCS and EHS. He concludes that �This strongly suggests that both [diseases] share a unique common pathophysiological mechanism,� (Belpomme 2015; Irigaray 2018).
Some physicians speculate that MCS and EHS are two manifestations of the same underlying illness (Brussels Declaration 2015; Belpomme 2015).
Much more speculative is a possible overlap with autism � especially the high-functioning version that is called Asperger�s. Autism is a spectrum illness where the symptoms and severity can vary dramatically. People with autism tend to be affected by various stimuli such as noise, smells, flickering lights, fluorescent light, and vibration that do not bother regular people. Many people have reached adulthood and had a thriving career in fields such as engineering and computer programming, despite having undiagnosed Asperger�s. These people also tend to be rather eccentric (Grandin 2015).
All of the above also characterize many people with EHS, as observed by this writer. The thought of a connection is compelling.
Then add that there are stories floating around about autistic children having fewer episodes when the radiation level is reduced (ClearLightVentures 2016). Some scientific reports (Herbert 2013; Mariea 2007; Mortazavi 2016; Alsaeed 2014) suggest that radio-frequency radiation could even be a cause of autism. Its rise did coincide with the wireless revolution.
Another speculative overlap is with ADHD (attention deficit hyperactivity disorder) as several people with EHS report similar symptoms when exposed to electromagnetic radiation. Such effects have been documented (Belyaev 2016; Thomas 2009; Havas 2004).
A pediatrician serving 800 Amish families says he has not seen a single case of ADHD in Amish children. The Amish are a religious sect who live without electronic gadgets, such as televisions and telephones. Some have no electricity at all (Ruff 2005).
Even more speculative are possible overlaps with restless leg syndrome, phantom vibration syndrome and �road rage.� As cars can emit powerful electromagnetic radiation, especially to the driver, it may be a trigger of road rage in some people (this author has measured car levels in excess of 100 milligauss/10 uT in ordinary gasoline-powered cars).
Children
EHS tends to mostly affect adults, but some children have it too. Even infants can have EHS (Belpomme 2015).
Children have a particular hard time with EHS, especially in school, since few schools are willing to accommodate their needs and peer pressure is relentless (G v. Fay 2017). This can have tragic consequences, such as when British teenager Jenny Fry committed suicide (Levy 2015).
Some parents have had to home-school their child or move to an area with a school that wasn�t focused on wireless gadgets (Ladberg 2010).
In Sweden there have been multiple summer camps for children with EHS, that were completely free of electronic gadgets. The children instead engaged in traditional activities, such as swimming, ball playing, and theatre (Ingram 2014).
Mobile phone base stations can apparently effect the behavior of sensitive children (Thomas 2009), and the mother�s use of a mobile phone can affect the child in the womb (Rezk 2008).

Exposure of pregnant women to mobile phones or magnetic fields could have health effects later on, including asthma and behavioral problems (Divan 2008; Divan 2012; Li 2011). Whether this is related to EHS is unknown.
Treatments
Research into treatments for EHS is still in its infancy. Since the illness is still considered controversial, funding is rarely available for researching treatments.
Medical treatments should rely on scientific knowledge as much as possible, but it would be cruel to tell EHS patients to wait decades before trying what appears to be helpful, despite lack of understanding. Even mainstream medicine relies to a large degree on �common practice� that is not actually based on solid science (Hardern 2003).
Some physicians focus on psychiatric and symptom treatments, despite that there is no scientific support for their effectiveness (Andersson 1996; Harlacher 1998; Hillert 1998). Also, patient surveys rate them thoroughly ineffective and sometimes even harmful (Belyaev 2016; Hagstrom 2013).
Avoiding or lessening exposures to EMF seems much more helpful, though it is not a cure (Belyaev 2016; Hardell 2022; Austrian Medical Association 2012; Genuis 2011; EI Wellspring 2018c; Hagstrom 2013; Marshall 2017; Solberg 2010; Roosli 2003).
A good start is to focus on the sleeping area. Keep in mind that most kinds of electromagnetic radiation pass through walls unhindered. Someone with EHS should not sleep near a refrigerator, electric meter, water heater, wireless phone, clock radio or any other appliance or electronics that is not fully disconnected.
Experiment by turning as much as possible off at night. Turning off the breakers lowers the electric field in the house and ensures all electronics is truly off � much electronics is not fully off even when their switches are in the �off� position.
Much electronics are a little better if run on batteries instead of grid power, as that eliminates one source of radiation (the power supply).
There is much advice on these things on the web. Some of that information is misguided, incomplete or based on myths. Use good judgement and experiment with simple and cheap measures before spending a lot of money and making major lifestyle changes.
Besides lowering exposures to EMF, treatment may focus on reducing the body�s load of mold, toxic chemicals, and heavy metals (Genuis 2011). Be aware that removal of heavy metals (chelation and amalgam removal) can be harmful if not done properly.
Since there is no standard treatment, patients sometimes experiment themselves. When someone reports feeling better the story spreads and others try the same treatment. It becomes popular for a while and then fades again as it was not the hoped-for cure. Such cycles have gone on for many years for all sorts of illnesses that have no cure, including tuberculosis, AIDS and cancer before effective treatments became available.
Various supplements are thought to be helpful, such as omega fatty acids, fermented papaya preparation, methylcobalamin B-12, N-acetyl cysteine and many others. Be aware that there is little science to support these, but the cost of trying them is usually moderate. Other treatments that some people have found helpful are �grounding� (�earthing�) and �brain retraining.�
Some people report relief after exposure by grounding themselves, such as when taking a shower, lying on grass or hugging a live tree.
We are not endorsing any specific treatments here, but are just listing some that appear to stay popular and have some rationale. Be aware that there are many unsupported ideas and even outright charlatans hawking miracle cures. Desperate people are easy prey, just look at the predatory pricing schemes the American health care and drug industries get away with.
EMF protection devices
A whole cottage industry of �EMF protection� devices has sprung up. These devices are sold with enticing promises of easy relief at a manageable cost. The advertising tends to be very vague about how they work, or invokes grand scientific terms but no actual substance (MWN 2010).
Some of these vendors say that they use patented technology, but having a patent means nothing. The patent office does not check if a device actually works, they only check if it is novel. There are lots of patents for perpetual motion machines and other devices that don�t work.
The U.S. Federal Trade Commission has issued a warning against these products, which it labelled �scams.� They suggest common-sense measures instead, such as limiting the use of mobile phones, etc. (FTC 2010).
Electrical sensitivity is not new
There were sporadic mentions of people unusually sensitive to electricity as far back as the 1870s. Early reports mostly involved operators of telegraphs and telephone switches. Later on came radar operators.
In 1971 scientist Zorach Glaser at the U.S. Naval Medical Research Institute published a list of symptoms associated with microwave use, along with an extensive bibliography.
In the 1980s computers were introduced by many businesses and the number of people having problems increased dramatically. The first EHS support group started in Sweden in 1987.
In 1988 about fifty telecom engineers got sick at the Ellemtel research center. The center accommodated them with shielded rooms and modified computers, but otherwise tried to keep the issue quiet, since it reflected poorly on their industry.
Research into EHS started around 1990 and focused on exposing volunteers to electromagnetic radiation to see what happened, but many of these studies were poorly designed and failed even to �prove� EHS existed. Very little research funding has been available to this day.
The scientific, social, and political history of EHS is covered in much more detail in documents available through a link at the end of this article (it also contains references to the above).
Who becomes electrically sensitive?
The scientific journals document cases across the industrialized world, including Canada, United States, Japan, Taiwan and several European countries.
Some studies have attempted to estimate how common the illness is:
|
California, USA |
3.2% |
Levallois, 2002 |
|
Stockholm |
1.5% |
Hillert, 2002 |
|
Switzerland |
5% |
Schreier, 2006 |
|
Colchester, UK |
4% |
Eltiti, 2007 |
|
Austria |
3.5% |
Schrottner, 2008 |
|
Vasterbotten, Sweden |
2.7% |
Palmquist, 2013 |
|
Netherlands |
7% |
Dongen, 2013 |
|
Netherlands |
4% |
Baliatsas, 2014 |
|
Taiwan |
4.6% |
Huang, 2018 |
Prevalence of electrical sensitivity in general population.
To what degree EHS exists in less affluent countries has not been studied and thus is unknown. The only documentation of EHS patients in such countries we have found is in Malaysia (Malek 2015).
The disease affects slightly more women than men, when looking at the general population (Levallois 2002; Hillert 2002; Roosli 2003; Schreier 2006; Dongen 2013).
However, one clinic specializing in environmental illness reports that two thirds of their patients are female (Belpomme 2015; Irigaray 2018). Surveys of patient support groups show they are dominated by women (FEB 2007; Schooneveld 2007; Kato 2012; Hagstrom 2013; Dongen 2013; Hojo 2016). This may mean that women tend to have the more severe version of electrical sensitivity.
The levels of sensitivity vary. One study found that 3.2 percent of Californians had some level of electrical sensitivity, while 0.5 percent were so strongly affected they had to change jobs or stop working entirely (Levallois 2002).
The illness affects people of all levels of education (Levallois 2002; Roosli 2003; Hojo 2016).
People in the age group of about 35 to 60 years old are much more likely to have EHS than younger or older people (Schreier 2006; Schooneveld 2007; Hojo 2016; Huang 2018).
The survey studies must be looked at with some skepticism. They were mostly telephone surveys asking people for their opinion, they did not rely on diagnosis made by trained physicians.
Celebrity patients
The World Health Organization started getting interested when their own Director-General, Gro Harlem Brundtland, announced she had EHS in 2002. She retired shortly after that. Before taking the helm of WHO Dr. Brundtland was prime minister of Norway for ten years (Dalsegg 2002).
The American model Jolie Jones, the Italian actor Lisa Granuzza Di Vita, and the British pop music guitarist Ricky Gardiner have gone public, as well as some Swedish authors. But they�ve largely been ignored by the media.
Impact on life
The impact on a person�s life can be rather mild, such as having to live with headaches or facial flushing when using a computer or mobile phone too much. At the other end of the spectrum the impact can be completely devastating. It can mean loss of career, breakup of family, loss of savings, and even homelessness.
The downward mobility can be quite steep. People can go from an affluent life to living in a camping trailer and dependent on the help of others in just a few months (Evans 2010; Ladberg 2010; Granlund-Lind 2004).
In a survey of 1732 Swedes with EHS, 79% stated they had a job prior to getting sick, while only 30% were able to continue working. In the same survey, 88% reported problems with fluorescent lights, 83% with computers without Wi-Fi and 62% with cars (this was before electric cars). Five percent responded that they lived partly, or wholly, without electricity (FEB 2007).
Some studies have looked at the employment rate of people with EHS. Since they are survey studies and recruited people in various ways, they are difficult to compare with each other.
|
Employed |
Country |
Source |
|
30% |
Sweden |
FEB, 2007 |
|
38% |
Holland |
Schooneveld, 2007 |
|
22% |
Norway |
Solberg, 2010 |
|
19% |
Japan |
Kato, 2012 |
|
38% |
Netherlands |
Dongen, 2013 |
|
63% |
Netherlands |
Baliatsas, 2014 |
|
38% |
Sweden |
Nordin, 2014 |
Employment rate of people with EHS

Mental health
Living with severe EHS can be like living with an abusive parent or spouse. Attacks can happen anytime with little or no warning. The abuser never takes any responsibility and often blames the victim. Complaints just invite more attacks.
When people�s lives are wrecked by an �accepted� illness, such as cancer, or by a catastrophe such as a burned-down home, they usually receive sympathy and support from many directions. Severe EHS can be just as devastating, but the victims often find themselves the subject of suspicion and sometimes even ridicule. Moreover, the source of the trauma continues, depriving the patient of a sense of feeling secure (Gibson 2016).
It is no wonder that some people with EHS become anxious and depressed, just as victims of domestic abuse tend to.
However, such effects might also be a direct effect of electromagnetic radiation acting on the central nervous system (Pall 2016).
Housing
Housing is a challenge for people with EHS. Apartments may not be feasible, due to the close proximity to neighbors and their electronic gadgets. The higher density of people can also mean a higher level of electromagnetic fields from the electrical wiring, wireless gadgets, etc.
If they can afford it, people with EHS tend to migrate to single-family homes. People with severe EHS may need to move to a rural area, with greater distances to neighbors and a lower level of electrosmog. A few people have to live in camping trailers and specially built houses (Granlund-Lind 2004; Evans 2010, 2019).
Daily Life
The daily life of someone with EHS can be as varied as for regular people. The level of sensitivity dictates many parts of the daily routine, however.
Some can cook on an electric stove, perhaps making sure to keep a distance when not tending the pot. Others cook very simple meals to minimize exposures, cook on a remotely controlled hot plate, on an outdoor propane stove, or have someone else do the cooking.
Some people can listen to a battery-powered radio for a few minutes to catch the news, while others can listen to music for hours.
Most people with EHS avoid using cell phones or use them sparingly. A traditional landline telephone is often their only viable means of communication. Some need to use a speaker phone to keep a distance to the telephone, while some use a special �tube phone.�
Computers are a common difficulty (FEB 2007). Some can only use a computer for five minutes, while others can use it much longer. In some cases, people live with the symptoms in return for being connected to the rest of the world a few times a week.
Access to medical clinics, dental clinics, hospitals, and nursing homes can be difficult (Granlund-Lind 2004; Evans 2010; Bryngelson 2014). Some places try to accommodate, but since modern medicine is now so dependent on electronics and wireless devices, it is difficult.
Transportation by cars, airplanes, buses, and trains can be very difficult (Granlund-Lind 2004; FEB 2007; Evans 2010; Kato 2012).
Most people with EHS do their own shopping, which means they get exposed to various sorts of radiation in the store from cell phones, cash registers, fluorescent lights, wireless networks, etc. Getting out of the house is good for the mental health and hiring a shopper is not always feasible. The exposures can be reduced by going when there are fewer customers and by keeping a distance to the radiation sources. It also appears that people with EHS can tolerate more radiation when moving around, compared to when at rest.
Some people with EHS have heightened sensitivities following trips out of their safe homes and may need a day of rest afterwards.
Daily living is often a matter of managing a budget of exposures. When the budget is exceeded, it has consequences. For some, this exposure budget is very small.
Social isolation
People with severe EHS are often socially isolated, since it is difficult to be around other people and go to public places due to the electronics that is everywhere (Granlund-Lind 2004).
Using public transportation can become impossible (FEB 2007; Kato 2012).
Asking people to not bring their portable electronics inside when they come to visit is often seen as an imposition. Visiting other people�s homes can be perilous, as people are often not even aware of all the electronics they have, and that much of it is still �on,� even when the device is turned �off.� And they may resent being asked to turn them off.
People with EHS may not be able to use a computer or a telephone and be isolated in that way as well. Few people are willing to correspond by letter anymore.
Some patients may rely on others for shopping and other chores outside the house and thus rarely go anywhere. This can also lead to a sense of loss of independence.
The controversy
Any new disease faces an uphill battle towards acceptance. Until a disease is accepted, its sufferers both have to live with a debilitating illness and with the effects of being labeled as �malingerers,� �hypochondriacs� and �psychosomatics� (Haas 2018; Caray 2017; Dodick 2008; Ware 1992; Ballweg 1995).
This is also the case for EHS sufferers (Genuis 2011; Ladberg 2010). On social media they are subject to hate and ridicule (EI Wellspring 2018a).
There are some studies on people with EHS done by psychologists. These tend to be strongly biased, and often with major mistakes that should appear obvious. Apparently none of them consulted people intimately familiar with EHS in the design and interpretation of the results.
The studies were clearly designed and done by people who had made up their minds that EHS was purely psychosomatic. There is nothing about �what if these people are right, what effects would that have on them?�
A standard error is comparing people with EHS to the general population, instead of people with other disabilities.
If they found people with EHS to be stressed and focused on their health, they automatically concluded that �caused� the EHS. They did not consider the impact of a difficult life-altering disability that carries a major stigma.
In one study (Donger) they made much of how member of an EHS support group were better educated, etc., than the general population. Again, they should compare with other support group members, not the general population.
They usually fail to consider that EHS can be mild or severe. The impact will vary accordingly, and perhaps how likely people are to join support groups.
The group around British psychologist Dr. James Rubin has published several papers to discredit people with EHS (Rubin 2005, 2011). They've even gone as far as claiming that the whole phenomenon is caused by media reports (Witth�ft 2012), and that people with EHS simply desire to withdraw from modern society and live like hermits (Boyd 2012) � a clear case of blaming the victims.
The American psychiatrist Joseph Pierre goes even further, accusing people with EHS of believing in the most outlandish conspiracy theories involving telepathic mind control and much else (Pierre 2022).
This writer has personally met over a hundred people with EHS. None of them had these ideas.
The problem with these psychiatrists seems to be that they only see people with EHS who also have psychiatric problems. And then they come to believe they are representative of the general EHS population. People who do not have psychiatric problems do not usually go visit a psychiatrist.
That is a repeat of the 1970s, where 90 percent of psychiatrists believed gay men were mentally disturbed, since that was what they saw in their clinics.
The lack of acceptance means people with EHS may be denied reasonable accommodations in medical facilities, denied disability pensions, and subjected to outright ridicule and hostility from families, officials and medical providers.
People labeled as mentally ill also get poorer service for other health needs (McCall 2010).
The stigma can force people to hide their disease as much as possible, which may mean suffering symptoms, lost productivity, poor job reviews, and eventual worsening of the illness and a lost job. The following is part of a public testimony in Sweden (Granlund-Lind 2004):
I have friends who work in healthcare � I won�t mention in which capacities � and when we meet in town we don�t greet one another. People at their workplace, the general hospital, are unaware that they are electro-hypersensitive � and they don�t dare mention it!
Many other now-accepted illnesses have gone through the same process, such as migraines, endometriosis, asthma, and multiple sclerosis. Autism used to be blamed on the mother not being affectionate enough and until recently stomach ulcers were believed to be caused by stress (EI Wellspring 2018b; Pall 2013).
Even sixty years after the first studies showed cigarettes could cause cancer, all the issues are not fully understood (Oreskes 2010).
The skeptics of EHS point to the lack of scientific research on EHS � research that is sorely lacking due to very little funding being available. Funding is very difficult to obtain for a controversial illness, which is kept controversial because there is so little science. It�s a vicious cycle. As Scientific American wrote: �Review panels, even when they are made up of excellent scientists, are allergic to risky ideas� and �Any idea that survives the scrutiny... has little chance of being truly disruptive or innovative. It must be mainstream...� (Ioannidis 2018).
Some detractors also point to the many and diverse symptoms people with EHS report and suggest it is impossible they all come from one source. Then consider that cigarettes are proven to cause two dozen diverse health effects, including heart disease, lung disease and low birthweight (CDC 2021; Oreskes 2010). Or that radium poisoning can result in tooth loss, joint pain, and anemia (Moore 2017). People with autism can also display a wide variety of symptoms and sensitivities (Grandin 2015).
Some point to the studies where people with EHS were exposed to electromagnetic radiation and could not tell the difference from a sham/placebo exposure (Rubin 2005, 2011). In some of the studies the test subjects could, in some they couldn�t. These kinds of tests are devilishly difficult to do, because of the complexities and diversity of people�s sensitivities, the need for strict environmental controls and for better selection of test subjects. We have yet to see any such test where they measured all the types of EMF that might be present. Some of those studies were like asking asthmatics whether they could detect a cigarette smoker in a room filled with cigar smoke.
These studies have been strongly criticized by many physicians (Genuis 2011; Belyaev 2016; Brussels Declaration 2015; Belpomme 2020, 2021).
One major problem is the lack of a good case definition to screen the participants in these studies. Most studies simply include anyone who believes they have EHS, despite that all the symptoms can have other causes. If people who are sick, but not with EHS, are included in the group of people believed to have EHS, that can greatly skew the results (Belpomme 2021; Leszczynski 2021). This is also a problem with the study of other �new� diseases, such as chronic fatigue syndrome (Tuller 2018).
It is also important to screen out participants who are traumatized by their illness, as they are probably not reliable testers. We are only aware of two studies that explicitly used such a screen (Sandstrom 1997; Irigaray 2018).
It has been suggested that people with EHS suffer from stress from using new technology (technostress) or get psychosomatic symptoms after hearing about health concerns in the popular media. A study of forty people with EHS in France found that just a few of them had even heard about any health effects before they got sick, and most had to search for an answer for a long time before they heard about EHS. Several were also technically savvy and thus unlikely to have �technostress� (Dieudonne 2016). This is also echoed in a detailed personal account of a computer engineer who took about a year to figure out his computer caused his headaches (Evans 2010).
When special interests are threatened by medical research, they tend to mount campaigns to keep the issue controversial in the eyes of the public. This has happened several times already, most notably with lead, asbestos and tobacco (Oreskes 2010; McGarity 2008). Special interests, especially the cell phone industry, have been very successful at keeping health effects from EMF controversial by funding research to cast doubt on the issue. Swiss researchers have shown that only 33% of industry-funded research finds any health effects, while 82% of independent research does show effects (Huss 2007). An investigative article in Microwave News found similar results (MWN 2006), as did one for power line studies (Carpenter 2019). An Australian study also confirmed this effect (Leach 2018). Funding for medical research is dominated by corporate sources. Scientists are well aware that if their results contradict corporate interests, their funding will likely disappear. This �funding effect� is well documented (Smith 2006; Bekelman 2003; McGarity 2008; Michaels 2008, 2020).
For more discussion see (Blank 2014; Davis 2010; EI Wellspring 2018b)
Much research is needed
Much basic research is needed to understand EHS�s complex pattern of symptoms and sensitivities, as well as the biological mechanism.
The disease still lacks a clear definition, an objective method of diagnosis and it is still debated whether it even exists as a legitimate illness.
Without a clear definition of who has EHS, it is difficult for scientists to compare their data and there is also a danger that people who do not actually have EHS are included in studies. Most studies simply include anyone who believes they have EHS, and who are willing to come to the scientist�s office. This may exclude the most severe cases and include people who actually do not have EHS but think they do.
Studies where EHS patients are exposed to electromagnetic radiation without knowing when it is on or off have turned out to be unreliable (Rubin 2005, 2011; Leszczynski 2021). The reasons are many, including improperly controlled environments and not giving the test persons enough time to recover (Belyaev 2016; Belpomme 2020; Genuis 2011). In one large study, 25% of the �EHS group� did not even react to any of the exposures (Rea 1991), so the choice of who to include in the �EHS group� is paramount.
Because of these types of studies are often unreliable, many scientists recommend not doing them until better methods are developed (Belyaev 2016; Brussels Declaration 2015). Even an editorial in the British Medical Journal frowns upon using such �placebo tests� in general (Spiegel 2004).
One standout study was done at Louisiana State University, where one person was tested a total of 450 times in a controlled setting and could accurately distinguish whether the equipment was on or not (McCarty 2011).
Critics have dismissed it by saying it is just one person. However, if something is supposedly impossible, then it takes just one well-documented example to prove that it is actually possible.
Much interesting research has already been done, as listed in this document, which needs to be followed up on. But the lack of funding prevents it. And many questions are still fully unexplored, such as whether there are links between EHS and Alzheimer�s, Parkinson�s, and various cancers.
Unfortunately, the lack of conclusive studies is sometimes used to paint people with EHS as psychosomatic and not suffering from a �legitimate� illness (Rubin 2005, 2011). This makes it more difficult to obtain research funding to resolve the issues.
Acceptance
The Austrian Medical Association is the only general medical society that has accepted EHS as a �legitimate� illness (Austrian Medical Association 2012).
In Sweden EHS is accepted as a �functional disability� which is more vague (Johansson 2010). In practice, Swedes with EHS are still discriminated against by many government agencies.
French courts have accepted EHS as �real� since 2015 (Le Monde 2015).
In 2011 the Council of Europe issued Resolution 1815 in support of people with EHS. The Council is an advisory body to the European Parliament (Council of Europe 2011).
The Bioinitiative Reports of 2007 and 2012 support people with EHS. They are produced by a group of independent scientists specializing in health effects from electromagnetic radiation (Sage 2007, 2012).
The EUROPAEM EMF Guideline 2016 report (Belyaev 2016) is the first attempt at suggesting radiation limits for people with EHS.
The World Health Organization has recognized the existence of EHS, but not formally accepted it by issuing an official diagnostic code � despite calls from the scientific community to do so (Brussels Declaration 2015; Hardell 2017a; Belpomme 2020).
In popular media
EHS has been featured in popular media. The TV series Better Call Saul (2015-2017) had a fictional character with EHS. The Netflix �docuseries� Afflicted (2018) featured one person with EHS. Both series falsely portrayed EHS as an imagined illness.
The Italian film Elettra is much friendlier. The main actor has EHS herself. The film is available for free, with English subtitles.
Communities
Some of the people with EHS have fled the electropollution in the cities and moved to rural areas, where a few informal communities have sprung up. These communities offer a way out of the social isolation and people who understand what we all have to go through. There is not the ongoing suspicion or need to keep reminding friends to turn off their wireless toys when visiting.
This is similar to veterans organizations, since only a fellow soldier can understand what serving in a war means.
The most famous EHS community is located around Green Bank, West Virginia, where most wireless devices are banned to protect a large radio observatory (Gaynor 2015).
Another large community is near the town of Snowflake, Arizona (EI Wellspring 2019). There are other communities around the American Southwest (Evans 2019).
In Europe there used to be a community in France (Abelous 2009). There is also one on an island off the coast of Sweden (they asked information about the location to be withheld).
Organizations
There are support groups and advocacy organizations across the world, including Australia, Britain, Canada, France, Germany, Spain, Japan, the United States and all the Scandinavian countries.
The oldest EHS organization was started in Sweden in 1987 and is still very active.
Activism
EHS organizations and individuals are demanding their civil rights in various countries. They have asked for safe access to medical facilities, fought against mobile phone base stations, against smart meters, and to retain telephone land lines. So far the successes have been few and modest.
As EHS is still falsely thought of as some sort of �anxiety� by many, it is difficult to be taken seriously. It is also difficult for the activists to show up in the halls of power, since the radiation levels there are likely to be rather high. With so many people with EHS so sick, it is difficult to get more than a handful to show up.

Picture courtesy Josh Hart/Stop Smart Meters!
The EHS community has not been active asking for funding for medical research. Funding is unfortunately very much a political process. According to surgeon Sherman Nuland, advocacy efforts were a major factor in increasing the budget for Alzheimer�s research 800-fold during the 1980s (Nuland 1993).
The EHS activists have still not learned to band together with other disability and patient groups for mutual support.
Recommended literature
The Non-Tinfoil Guide to EMFs, Nicolas Pineault, N&G Media, 2017.
The Invisible Rainbow: a history of electricity and life, Arthur Firstenberg, Santa Fe: AGB Press, 2017.
Overpowered: what science tells us about the dangers of cell phones and other WiFi-age devices, Martin Blank, Seven Stories Press, 2014.
Forced to Disconnect: Electrohypersensitive Fugitives in Sweden, Gunilla Ladberg, 2010. (Available for free download, originally published in Swedish).
Chemical and Electrical Hypersensitivity � A Sufferer�s Memoir, Jerry Evans, McFarland, 2010.
The Invisible Disease, Gunni Nordstrom, O-Books, 2005.
Black on White: Voices and Witnesses about Electro-Hypersensitivity, Rigmor Granlund-Lind and John Lind, Mimers Brunn, 2004.
Cross Currents � The Perils of Electropollution, Robert O. Becker, M.D., Tarcher, 1990.
More information
A wide variety of articles about how to cope with EHS is available on www.eiwellspring.org.
For articles about the history of EHS, including scientific, social, and political milestones, www.eiwellspring.org/ehshistory.html.
For personal stories go to www.eiwellspring.org/facesandstories.html.
References and notes
The list of references is in a separate file: www.eiwellspring.org/health/IntroductionToEHSreference.htm
2008 (updated 2024)